Why kidneys matter — structure, function, prevention & treatment
The kidneys are among the most vital organs of the human body. Malfunction of the kidneys can lead to serious illness or even death. Each kidney has a very complex structure and function.
They have two important functions namely: to flush out harmful and toxic waste products and to maintain balance of water, fluids, minerals and chemicals i.e., electrolytes such as sodium, potassium, etc.

Structure of the Kidney
How kidneys work
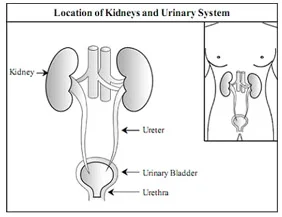
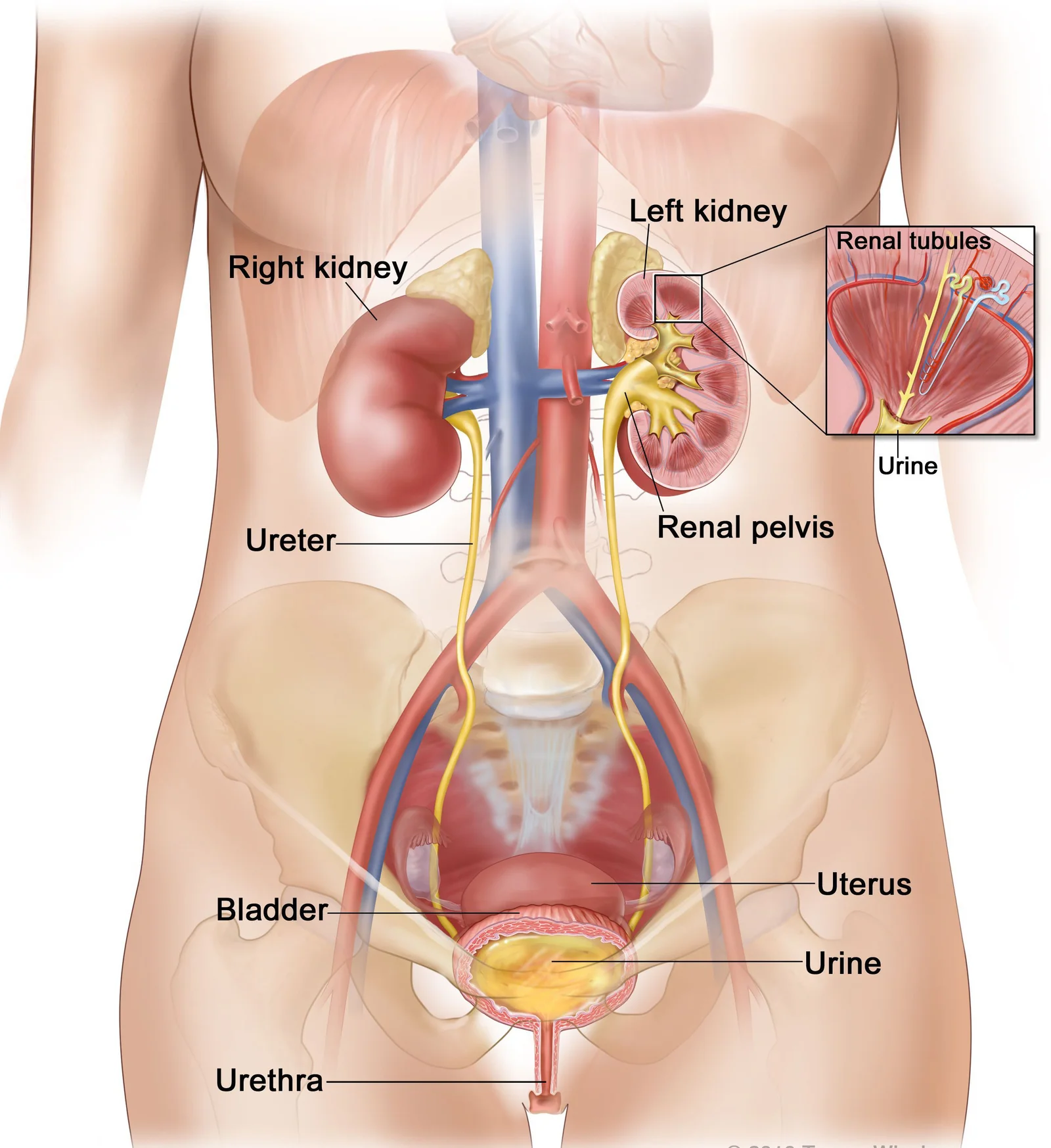
The kidney produce urine by removing toxic waste products and excess water from the body. Urine formed in each kidney passes through the ureter, flows into bladder before finally being excreted through the urethra.
Most people (males and females) have two kidneys. The kidneys are located at upper and back side of the abdomen, on either side of the spine. They are protected from damage by the lower ribs. The kidneys lie deep inside the abdomen so normally one cannot feel them.
The kidneys are a pair of bean shaped organs. In adults, a kidney is about 10 cm long, 6 cm wide and 4 cm thick. Each kidney weighs approximately 150-170 grams.
Urine formed in the kidneys flow down to urinary bladder and then through the ureters. Each ureter is about 25 cm long and is a hollow tube- like structure made up of special muscles.
The urinary bladder is a hollow organ made up of muscles, which lie in the lower and anterior part of the abdomen. It acts as a reservoir of urine. The adult urinary bladder hold about 400-500 ml of urine; when filled to near capacity, a person feels the urge to pass urine.
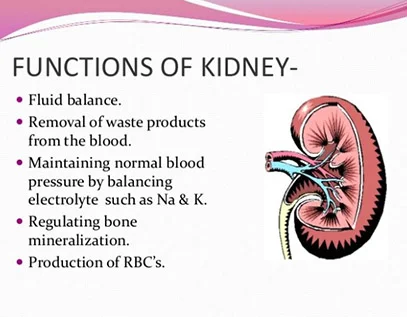
Functions of the kidney
Each kidney carries out the essential job of flushing out harmful and toxic by-products. At the same time, they also regulate and maintain the right balance and levels of water, acids and electrolytes.
The urine in the bladder is excreted through the urethra during the process of urination. In females, the urethra is relatively short, while it is much longer in males.
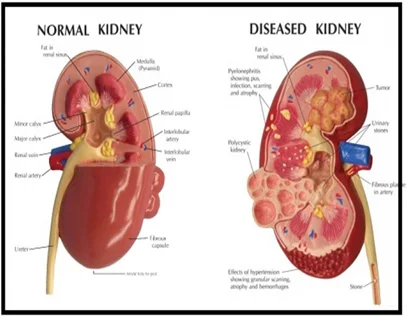
Major Kidney Disease
Common Conditions
- Kidney failure – Acute renal failure and chronic kidney disease
- Urinary stone diseases
- Urinary infection
- Uncontrolled blood pressure and kidney disease
- Diabetes related kidney disease
- Kidney disease in children
Kidney Failure Overview
Kidneys are no longer able to remove waste effectively from the body to balance fluids. The build up of waste products can change the chemistry of your body causing symptoms.
There are two types of kidney failure:
- Acute kidney failure
- Chronic kidney disease
Acute Kidney Failure
Acute means the kidneys have failed suddenly, often due to infections, a toxin (a drug allergy or poison) severe dehydration or blood loss. This type of kidney failure is usually temporary. If the cause is treated, the kidneys may be able to recover some or all of their function.
Chronic Kidney Failure
Chronic kidney failure (chronic kidney disease) occurs when kidneys not able to perform their functions to full capacity. This can happen all of a sudden or over time. Gradual progressive and irreversible loss of kidney function over several months to years leads to complete kidney failure.
Prevention of Kidney Disease
Kidney diseases are silent killers. They may cause progressive loss of kidney function leading to kidney failure and ultimately requirement of dialysis or kidney transplant to sustain life. CKD is very common and has no cure, so prevention is the only option. Early detection and treatment can often keep CKD from getting worse, and can prevent or delay the need for definitive therapy.
How to prevent kidney diseases?
Never ignore your kidneys. Important aspects about care and prevention of kidney diseases are discussed in the following categories:
Precautions for Healthy Person
Seven effective ways to keep the kidney healthy:
Kidney diseases are often silent diseases and do not produce any symptoms until they reach an advanced stage. The most powerful and effective but, sadly, underutilized method for early diagnosis and prevention of kidney disease is a regular kidney check-up.
Annual kidney check-up is a must for high risk persons who suffer from diabetes, high blood pressure, obesity or have a history of CKD in the family. If you love your kidneys (and, more importantly, yourself), do not forget to get a regular kidney checkup after the age of 40. A simple method for early detection and diagnosis of kidney disease is at least an annual blood pressure measurement, urinalysis and a test to measure creatinine in blood.
Precautions for Kidney Patients
Click on each precaution to learn more:
For all diabetic patients, prevention of kidney disease is particularly essential because diabetes is the leading cause of CKD and kidney failure throughout the world. About 45% of new cases of end-stage kidney disease (ESKD) are due to diabetic kidney disease (DKD).
For early diagnosis of diabetic kidney disease, a simple and effective way is at least a tri-monthly measurement of blood pressure and urinalysis to check for the presence of protein or microalbuminuria (MA) by dipstick. This is the best and ideal test for the earliest diagnosis of diabetic nephropathy, which should be done every year. Measure serum creatinine (and estimated glomerular filtration rate, eGFR) to assess kidney function at least once every year.
High blood pressure, presence of protein in the urine, generalized swelling, frequent fluctuations of blood sugar readings, reduction in insulin requirements and appearance of diabetic eye disease (diabetic retinopathy) are important clues to kidney involvement in the presence of diabetes. Beware of these danger signals and consult your doctor immediately.
To prevent DKD, all diabetics should control diabetes meticulously, maintain blood pressure less than 130/80 mmHg (Angiotensin Converting Enzyme inhibitors, ACE-I or Angiotensin Receptor Blockers, ARB are the preferred antihypertensive drugs), reduce the amount of protein in their diet and control lipids.
Hypertension is the second most common cause of CKD. As most people with high blood pressure have no symptoms, many hypertensive patients tend to become non complaint with prescribed treatment or some may even discontinue treatment altogether. Some would discontinue treatment as they feel more comfortable without medicine. But this is dangerous. Uncontrolled hypertension for a prolonged period of time can lead to serious problems like CKD, heart attacks and strokes.
To prevent kidney disease, all hypertensive patients should take regularly prescribed blood pressure medications, get their blood pressures checked regularly and consume a proper diet with appropriate salt restriction. The goal of therapy is to keep the blood pressure less than or equal to 130/80 mmHg. For early diagnosis of kidney damage all hypertensive patients should check urine and blood creatinine every year.
CKD is a non-curable disease. But early detection and diagnosis and subsequent dietary restrictions, regular follow up and proper treatment will slow down its progression and may potentially postpone imminent requirement of dialysis or kidney transplantation.
Round the clock proper control of high blood pressure is an effective measure to prevent progression of CKD. It is highly recommended to keep blood pressure 130/80 mm Hg or below. The best way to attain good control is to monitor the blood pressure regularly at home and maintain a chart, which would immensely help the doctor in adjusting the blood pressure medications accordingly. In patients with CKD, factors such as hypotension, dehydration, urinary tract obstruction, sepsis, nephrotoxic drugs etc. need to be promptly identified. Prompt management of these factors may lead to maintenance of stable kidney function, and at times, even improvement in kidney function.
Diagnosis of Kidney Diseases
High risk for kidney problems
Chronic kidney disease (CKD) is not curable and if not treated can lead to end stage kidney disease (ESKD). However, if diagnosis is made early, appropriate medical treatment can be rendered and progression to ESKD can be delayed or slowed. So whenever a kidney problem is suspected, it is advisable to go for immediate check-up and early diagnosis.
Who should get their kidneys checked?
Anyone can develop a kidney problem, but the risk is higher in the presence of these symptoms or factors:
Screening in such high risk individuals helps in early detection and diagnosis of kidney disease. Early stages of chronic kidney disease are usually asymptomatic, laboratory tests are the only way of detection.
Urine Examination
The most important first step in detection:
- Albumin/Protein: Essential to check if kidneys are leaking protein.
- Microscopy: To check for red blood cells or infection.
Blood Tests
Tests to measure kidney function efficiency:
- Creatinine and Urea: To assess waste removal efficiency.
- Hemoglobin: To check for anemia (low blood count).
- Electrolytes: To check sodium, potassium, etc.
Radiological Tests
Imaging helps visualize the kidney structure:
- Ultrasound/KUB: Essential for checking size, stones, or cysts.
Treatment of Chronic Kidney Disease
Medical Management is Key
"Early detection and meticulous conservative medical management is the only feasible and less expensive way to manage CKD and delay the need for dialysis or transplant."
Importance and Goals
The three treatment options for CKD are medical management, dialysis, or transplant.
- All patients start with medical management (medicine, diet, and monitoring).
- Advanced stages (ESKD) require kidney replacement (dialysis or transplant).
The Reality in India
Advanced CKD requires expensive dialysis or transplant. In India, due to cost and availability, only 5-10% of kidney patients receive these treatments, while the rest may perish without definitive therapy. Early management is critical.
Goals of Management:
- Slow down the progression of the disease.
- Treat underlying causes and contributing factors.
- Relieve symptoms and treat complications.
- Reduce cardiovascular disease risk.
- Delay the need for dialysis or transplant.
Lifestyle & General Measures
These measures are vital for reducing overall health risk:
- Stop Smoking: A critical step to prevent further vascular damage.
- Weight & Exercise: Maintain a healthy weight and remain physically active.
- Alcohol Intake: Limit consumption to reduce metabolic strain.
- Healthy Eating: Follow a structured plan and reduce salt intake.
- Medication Adherence: Take all medications exactly as directed; they are adjusted based on your kidney function.
- Specialist Follow-up: Regular check-ups with a nephrologist are mandatory for monitoring.
Caution: Because many early CKD patients are asymptomatic, families often fail to recognize the seriousness and stop treatment. Discontinuing therapy leads to rapid worsening.
Dietary Restrictions in CKD
Dietary needs vary by severity. Following these restrictions strictly helps manage symptoms and slow disease progression.
Salt restriction is advised to control high blood pressure and swelling.
- Do not add extra salt to food at the table.
- Avoid: Fast food, papad, pickles, and most canned/processed foods.
Decreased urine volume in CKD patients causes fluid buildup.
- Fluid restriction is advised for all CKD patients with swelling.
- In severe cases, excess fluid can cause life-threatening breathlessness.
Blood potassium levels often rise in CKD, which can stop the heart. Restriction is life-saving.
- Avoid/Restrict: Dry fruits, coconut water, potatoes, oranges, bananas, and tomatoes.
High-protein diets can accelerate the rate of kidney damage.
- Patients should follow a low-protein diet as prescribed by their nephrologist to preserve remaining kidney function.
Dialysis — Meaning & Indication
Meaning and Indication
Dialysis is a procedure by which waste products and excess water that accumulate in renal failure are removed from the body artificially. It is a life-saving technique for patients with End Stage Kidney Disease (ESKD) or Acute Kidney Injury.
How Dialysis Helps
- Purification: Removal of waste products such as creatinine, urea, etc.
- Fluid Balance: Removal of excess fluid and maintenance of water balance.
- Chemical Balance: Correction of electrolyte and acid-base disturbances.
Note: Dialysis cannot replace hormonal functions like erythropoietin production.
When is dialysis needed?
When kidney function reduces by 85-90% (ESKD), toxins like creatinine and nitrogenous waste build up, leading to nausea, fatigue, and breathlessness (Uremia). At this stage, medical management becomes inadequate and dialysis is required.
Can dialysis cure CKD?
No. CKD is irreversible; ESKD requires lifelong dialysis unless a transplant is performed. However, for AKI (Acute Kidney Injury), dialysis may only be needed temporarily until function recovers.
Types & Process of Dialysis
Click to explore the detailed procedures:
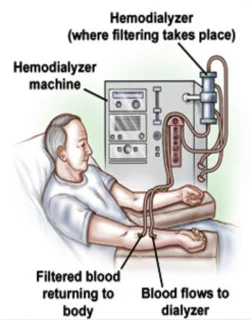
In HD, blood is purified by passing it through a dialyzer (artificial kidney) aided by a machine. Usually performed in hospitals 3 times per week for ~4 hours each.
- Machine pumps blood from the body to the dialyzer through flexible blood tubings.
- Heparin infusion or continuous saline flushing is done to prevent clotting of blood.
- The dialyzer (artificial kidney) is a special filter which removes extra fluids and waste products.
- Vascular Access: Done via Central Venous Catheters, Native Arteriovenous (AV) Fistulas, or Synthetic Grafts.
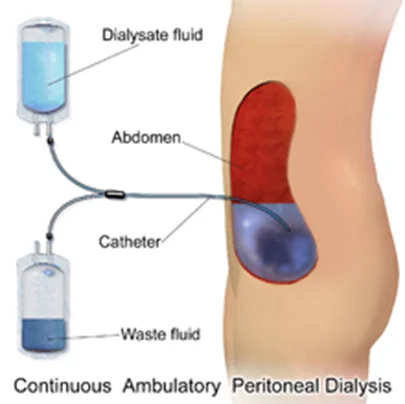
PD uses the peritoneum (abdominal lining) as a natural filter. A soft catheter is inserted into the abdominal cavity to infuse dialysis solution.
- Can be done at home, often without a machine.
- Mechanism: Toxins pass from the blood into the solution through the peritoneal membrane.
- Types:
- Intermittent Peritoneal Dialysis (IPD)
- Continuous Ambulatory Peritoneal Dialysis (CAPD)
- Continuous Cycling Peritoneal Dialysis (CCPD)
Kidney Transplant
Kidney transplantation (KT) is the outcome of great advancement in medical science. It is the treatment of choice for end-stage kidney disease (ESKD). Successful kidney transplantation may offer better quality of life and longer patient survival compared with dialysis. Life after successful kidney transplantation is almost normal.
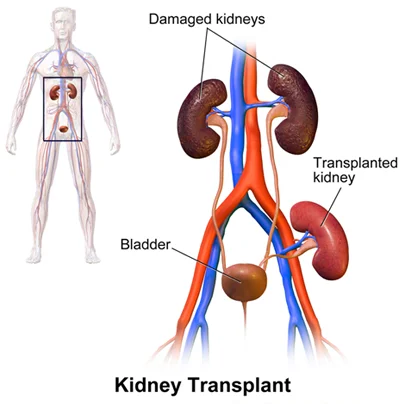
What & When?
Kidney transplantation is a surgical procedure where a healthy kidney (from a living or deceased donor) is placed into a person suffering from ESKD. It is necessary for patients on dialysis or those approaching ESKD (pre-emptive KT).
When is it NOT required?
A patient with acute kidney injury should not undergo KT. It is also not done if only one kidney fails and the other is still functioning. Transplantation should only be done if the renal failure is irreversible.
The "Gift of Life"
Dialysis replaces only a portion of kidney filtration. Transplantation addresses more functions (hormonal, etc.) and offers complete rehabilitation. As it saves lives and enables a near-normal life, it is often called the “Gift of Life”.
Major benefits of a successful kidney transplant include:
- Better Quality of Life: Almost normal and active lifestyle with higher energy levels.
- Freedom from Dialysis: Avoid costs, time loss, and complications associated with dialysis.
- Longer Life Expectancy: Transplant patients generally live longer than those staying on dialysis.
- Fewer Restrictions: Significantly lesser dietary and fluid restrictions.
- Cost-Effective: While initial cost is high, long-term expenses (after 2-3 years) are lower than maintenance dialysis.
- Personal Well-being: Improved sexual life and higher chances of starting a family.
Living Donor
A healthy kidney from a living person. Humans can live perfectly normal lives with one healthy kidney, allowing them to donate to a family member or loved one.
Deceased Donor
Someone who consented to organ donation upon death (cadaveric). Requires placement on a waiting list, which can take several years. Regular blood tests are needed while waiting.
Who can donate?
Typically blood relatives (parents, siblings, children) or non-blood relatives (husband/wife).
Advantages of Living Donation
- Living donor kidneys usually last longer than deceased donor kidneys.
- Surgery can be planned to suit both donor and recipient schedules.
- Reduced risk of rejection, especially with blood relative donors.
Pre-Transplant Steps
- Voluntary Consent: Willingness of the donor.
- Medical Evaluation: Thorough history, physical exam, lab, and radiological check for fitness.
- Legal Permission: Approval from the official Authorization Committee.
Paired Kidney Donation
Used when a relative is willing to donate but isn't a match. In a "swap," your relative donates to another recipient, and their relative donates to you.
ABO Incompatible Transplants
Specialized methods allow for successful transplantation even when blood types don't match, by making the recipient's body less sensitive to the incompatible blood type.
Contact & Resources
Dr Bhavin Brahmbhatt — Consultant Nephrologist & Transplant Physician at Sovin Kidney Clinic
Sovin Kidney Clinic
G 14/15, Race Course, Near MLA Hostel
Phone: 9548658489